A 57 year old female with acute gastroenteritis with prerenal AKI
UNIT 4 ADMISSION:
A 57 year old female resident of nalgonda , home maker came to casuality with complaints of:
- Fever since yesterday evening
-loose stools since yesterday night
HOPI:
Patient was apparently asymptomatic 1 day ago. Then she developed fever which is high grade , intermittent, associated with chills since yesterday evening. Subsided with medication .
C/O loose stools 4 to 5 episodes , watery in consistency since yesterday night.
No c/o pain abdomen, vomitings .
No h/o passage of blood /black stools.
No h/o bleeding gums , petechiae , red urine, burning micturition .
No h/o outside food consumption .
Past history:
k/c/o DM type 2 since 8 years .( on unknown medication) .
Not k/c/o HTN, TB, Asthma, CAD, CVA
Personal history :
She is married .
Diet: mixed
Appetite: lost
Sleep: Adequate
Bowel and bladder : regular
Addictions: no addictions
O/E:
Pt is conscious, coherent , oriented to time , place , person
No pallor, Icterus, cyanosis, clubbing, lymphadenopathy , edema
Temp- 98.6°F
BP-80/60 mm of hg
PR- 153/min
RR- 24/min
Spo2- 95%at RA
Grbs- 300 mg/dl
Systemic examination:
CVS:
s1 s2 present , no murmurs
RS:
BAE present, NVBS
P/A:
Soft, non tender
Bowel sounds present
CNS:
Intact
Provisional diagnosis:
Acute gastroenteritis with prerenal AKI
Investigations:
On 05/09/21:
Hemogram:
Hb- 11.7
TLC- 11,200
PLT- 1.88
RFT:
Blood urea- 48
Sr. Creatinine- 1.8
Na+ : 134
K+ : 4.2
Cl- : 101
LFT:
TB- 0.87
DB- 0.20
AST- 33
ALT- 19
ALP- 104
Sr. Protein- 5.1
Uric acid: 5.4
RBS : 375
Serology: Negative
CUE:
Sugars- nil
Albumin- nil
Rbc- nil
Epithelial cells- 2 to 3
Pus cells- 2 to 3
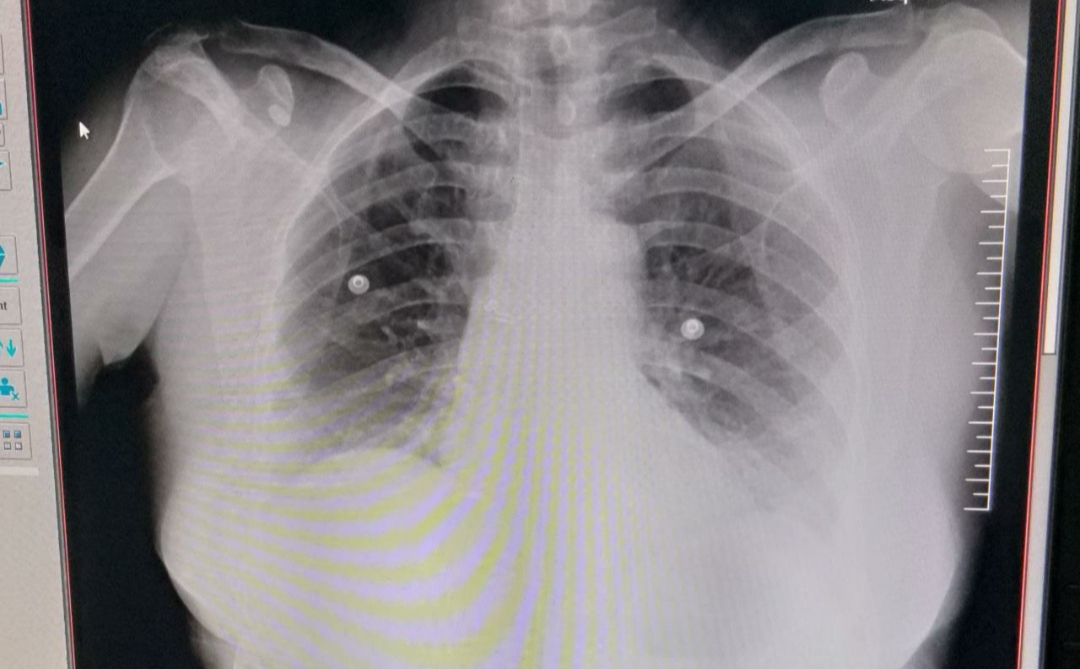
Chest xray:
Xray abdomen:
Ultrasound:
Ecg:
On 06/08/21:
Hemogram:
Hb- 11.7
TLC- 12300
PLT- 1.62
On 07/08/21:
Hemogram:
Hb: 10.1
TLC: 10400
PLT: 1.56
Serum electrolytes:
Na+ : 139
Cl- : 106
K+: 3.1
On 08/09/21:
Hemogram:
Hb- 10.6
TLC- 9000
PLT- 1.85
SR. ELECTROLYTES:
Na+ : 142
K+ : 3.1
Cl- : 105
Treatment given:
Day1:
1. Plenty of oral fluids
2. IVF - NS, RL, @ 100 ml/ hr
3. Inj. Pan 40 mg IV OD
4. Inj . Zofer 4 mg IV BD
5. Inj. Ceftrioxone 1 gm IV BD (Day 1)
6. Tab pcm 650 mg po sos
7. Monitor vitals 4th hrly
8. GRBS charting 8th hrly
9. Strict I/o charting
10. Tab ultracet 1/2 tab po BD
Day 2:
1. Plenty of oral fluids
2. IVF - NS, RL @100ml/ hr
3. Inj. Ceftrioxone 1 gm IV BD (day 2)
4. Inj. Pan 40 mg iv od
5. Inj. Zofer 4 mg iv sos
6. Non diabetic ors sachets
7. Tab Redotil 100 mg po BD
8. Tab pcm 650 mg po sos
9. Tab ultracet 1/2 tab po BD
10. Monitor vitals 4th hrly
11. GRBS charting 6th hrly
12. Strict I/o charting
13. Inj . HAI sc
Day 3:
1. Plenty of oral fluids
2. IVF - NS, RL @100ml/ hr
3. Inj. Ceftrioxone 1 gm IV BD (day 3)
4. Inj. Pan 40 mg iv od
5. Inj. Zofer 4 mg iv BD
6. Non diabetic ors sachets once
7. Tab Redotil 100 mg po BD
8. Tab pcm 650 mg po sos
9. Tab ultracet 1/2 tab po QID
10. Monitor vitals 4th hrly
11. GRBS charting 6th hrly
12. Strict I/o charting
13. Inj HAI sc
14. Syp potchlor 10 ml po OD
15. Inj. Metrogyl100 ml Iv tid(Day 1)
Day 4:
1. Oral fluids with ORS sachets (non diabetic )
2. IVF - NS , RL @100ml/hr
3. Inj. Pan 40 mg IV OD
4. Inj. Zofer 4 mg IV BD
5. Inj. Metrogyl 100 ml IV TID
6. Syp. Potchlor 10 ml po BD
7. Tab PCM 500 mg po sos
8. GRBS 6th hrly
9. Inj . HAI sc